Primary Care Networks are still in the early stages of formation and many people may be unaware or have little knowledge of them.
Primary Care Networks were introduced in the NHS Long Term Plan in 2019 and since then, there has been the beginning of many formations to collaborate healthcare services for the benefit of patients and their healthcare.
Since the introduction of the NHS’s Long Term Plan, practices have organised themselves into their Primary Care Networks as of 15th May 2019 and all except a handful of GP practices in England have come together, resulting in around 1,300 geographical networks (Kings Fund, 2019, https://www.kingsfund.org.uk/publications/primary-care-networks-explained).
Aiming to collaborate a workforce and form a more inclusive work environment to better the needs of patients, the particular challenges, risks and successes of these formed Primary Care Networks can be evaluated.
Questioning ‘are primary care networks a challenging collaboration?’, this article will provide a holistic overview of primary care networks, the potential risks and challenges and finally, the successes.
What are Primary Care Networks?
A Primary Care Network is one or more general practice’s working collaboratively together. This usually consists of networks of doctors and other healthcare providers such as dieticians, pharmacists and nurses.
Primary Care Networks ‘form a key building block of the NHS long-term plan’. Whilst there were some different ways of working together before the introducing of PCN’s, they aim to create a formal structure.
How are Primary Care Networks formed?
As stated on the King’s Fund, networks are geographically based and cover all practice within a clinical commissioning group boundary.
It is not a requirement that primary care networks are formed, but if practices choose not to join, they will lose out on significant funding. It’s also important to note that occasionally, a single practice can function as a network if they meet the size requirements. PCN’s will receive funding to employ additional health professionals such as pharmacists and paramedics to enable a greater formation.
Why were Primary Care Networks introduced?
The NHS were facing issues with increased demand in healthcare services. Patients were living longer, with more complex and long-term health conditions. These issues were also coupled with an understaffed workforce.
As a result, the introduction of Primary Care Networks aimed to alleviate the strain on healthcare staff, allowing them to work together to deliver primary care services.
The introduction of Primary Care Networks aimed to ‘build on the core of current primary care services’ enabling a more pro-active and co-ordinated workforce.
Primary Care Homes (introduced in 2015) were an approach to strengthening primary care. The model brings together a range of health and social care professionals to work together to provide enhanced personalised and preventative care for their local community.
On 31st March 2017, NHS England publishes ‘Next Steps on the NHS Five Year Forward View’, which reviewed the progress made since the launch of the ‘NHS Five Year Forward View’ in October 2014. The revised Five-Year Forward View set out ‘practical and realistic steps’ to ensure the delivering of a more responsible and sustainable model.
Healthcare professionals were encouraged to work together, in networks of 30,000-50,00 patients, which built on the Primary Care Home model. Following this, in February 2018, refreshed ‘NHS Plans for 19’ was introduced. This plan set out the plans for CCG’s, encouraging every GP to be part of a PCN so that these could cover the whole country as far as possible by the end of 2018/2019.
The GP contract, agreed in January 2019, is a new extension part of NHS England’s five-year framework for GP services, named the ‘Network Contract Directed Enhanced Service’ (DES). This contract went live on 1st July and enables GP practices to ‘play a leading role in every PCN’.
As part of this contract, the DES announced that PCN’s must appoint a clinical director as their named leader, responsible for delivery. The network agreement states the rights and obligations of the GP practices within the network, how the network will partner with non-GP’s, and a patient data-sharing requirement.
Here are some key legislative dates as mentioned above:
2015: The National Association of Primary Care (NAPC) launched the Primary Care Home model at their annual conference
April 2016: NHS England introduced GP Five Year Forward View
2nd February 2018: NHS England introduced ‘Refreshing NHS Plans for 19’
7th January 2019: NHS Long Term Plan introduced
31st January 2019: GP Contract 2019/20 (outlines what PCN’s will be)
15th May 2019: Practices have to organise themselves into networks and submit signed network agreements to their clinical commissioning group (CCG).
1st July 2019: NHSE expects the network contract to provide 100% geographical coverage
Benefits of Primary Care Networks
As previously mentioned, PCN’s were introduced to allow GP and primary care services to scale up by grouping. As a PCN, workforces can team up to deliver as a larger entity and pull resource where needed.
PCN’s have the potential to substantially improve patient experience. One of the many benefits is that the accessibility of healthcare services increases, allowing them to have access to extended services.
In terms of other benefits, each PCN will encounter their own set of benefits individually. As provided below, success stories present two different sets of benefits for patients and staff.
Examples of these benefits as outlined in the success stories are:
- Better work relationships and collaboration
- A stronger focus on patient care and experience
- Easier to identify key issues within the community through collaboration
Dr Nikki Kanani, a London GP and NHS England’s acting medical director for primary care stated: “people across the country will benefit from access to more convenient and specialist care through their local GP. As part of the long-term plan for the NHS, GP surgeries large and small will be working together to deliver more specialist services to patients”- Guardian.
Risks and Challenges of Primary Care Networks
As health.org.uk and Nuffield Health outlined, there are a particular set of risks and challenges associated with PCN’s:
1. Speed
One of the most prominent risks of PCN’s is the speed of implementation of these collaborations. With such a tight set of deadlines associated with PCN’s, it may be difficult for people to familiarise themselves with PCN’s and then form their practices into networks within these time restraints.
As Nuffield Health illustrated, these tight deadlines could mean that failure was inherent form the policy design. It could be said that these timescales are unrealistic and ambitious, not giving professionals enough time to adjust to the rapid changes.
2. Funding
In terms of deciding not to join a network, practices will miss out on the sources of funding. However, even if there is a formation of a PCN, there is a risk that there will be a removal of other sources of income for practices.
In addition to this, NHS England has promised to meet 70% of costs of employing most additional staff need for the PCN, meaning networks must cover the remaining 30% of the cost associated with this. This could be particularly costly for those practices that cannot afford this.
3. Workforce and workload
A particular risk associated with PCN’s is that they may decrease the amount of GP time available.
Additionally, there is no proof that the NHS is supplying 20,000 additional health professionals as stated in their plan. Increasing this workforce also means accommodating for these new staff members, which may pose a particular challenge for some GP’s where workspace is limited.
There could be a lack of operational support to realise the amount of PCN roles that need to be filled in this short time period. Additionally, some practices may not have the funding available to appoint new staff members.
4. Lack of collaboration
There is a risk that PCN’s may not be able to form effective organisations.
The knock-on effects of the lack of collaborations between practices are that there are disputes which could result in isolation and resist, creating further issues amongst networks. Thus, this could result in a lack of collaboration and the failure of an effective network model.
As stated on the King’s Fund website, the research found that collaboration in general practice was most successful when it had been generated organically over several years and if it was reinforced by trust, relationships and support. On the other hand, research has shown that a lack of clarity of purpose and engagement or over-optimistic expectations resulted in less effective collaborations. This suggests that collaboration and focus should be coupled together to form an effective PCN.
5. Lack of focus
There are a large number of objectives for PCN’s. The number of objectives that professionals must fulfil, may be unrealistic and put further pressure on them.
In 2020/21, there are five out of seven service specifications expected to be delivered. This heightened pressure on healthcare professionals may result in intolerable pressure resulting in a lack of focus.
Protecting Risks and Challenges of Primary Care Networks
Although, as Primary Care Networks are still in the early stages of development, these risks and challenges could be easily rectified at this early stage.
Nuffield Health provides a series of possible solutions to these problems, some of which are provided as examples below:
Issue: Lack of collaboration/ not able to create effective organisations
Possible Solutions:
- Create a new vision for primary care: defining what an effective PCN looks like and what can be achieved.
- Carve out time (using paid backfill, ideally from CCG’S/STP’s) to build a shared organisational vision
- Draft vision statements as practical documents
- Create clear roles for each of the different levels of the local system
Issue: Lack of focus
Possible Solutions:
- ‘Work with CCG’s and commissioning support units to undertake multi-level approaches to tackling population health and general operations’
- ‘share learning across practices and governance levels in a neighbourhood to create a sense of shared ownership’
Issue: Speed
Possible Solutions:
- ‘Policymakers should acknowledge that an organisational plan can take up to two years, and outcomes 5-10 years to realise’
- ‘STPS/ICSs and CCGs should work closely with PCNs to agree roles, responsibilities, development plans, timelines and funding arrangements until 2025’
- ‘PCNs leads and practice liaisons should jointly agree on the purpose of new roles and their contractual terms and conditions’
- ‘CCGs should examine where their management support should be best placed- this role has had little attention to date in primary care workforce planning and funding’
Issue: Workforce/ Workload
Possible Solutions:
- ‘create a shared physical space for the PCN and bring people together during their working day to talk about what they want to achieve’
- ‘help clinical directors to improve the capacity and capability of their network by focusing initially on small, achievable initiatives that help or reduce workload in individual practices and build trust’
- ‘Appoint leaders who have skills to make sense of the environment and set the direction, as well as managing the many different aspects of the organisation’s functions’
Successes of Primary Care Networks
Despite the foreseeable risks and challenges to PCN’s, there have been a number of success stories which illustrate the impact that they have already made.
Yorkshire Primary Care Network
A success story on the NHS Confederation website discusses how a Yorkshire Primary Care Network bridged the gap between health and social care by linking up care in their region.
They sought to identify the problems that their patients had and work towards rectifying these issues as a PCN. One of the issues identified was that they had a considerably high percentage of older patients and they had to be attentive when caring for those patients, especially those who were on a terminal decline. Thus, they appointed a care co-ordinator and benefitted from the PCN team across the network.
Alongside this, a Parkinson’s nurse was appointed, a partnership with the York Teaching Hospital has been formed and a rapid cancer diagnosis pathway is underway.
Dr Evans, one of the doctors in the Yorkshire Primary Care Network stated: “The care of our patients is a lot more organized and anticipatory, and [there is] less crisis. But actually, more important, it works”
Chester East Primary Care Network
Chester East Primary Care Network who cover a network population of 37,020 patients.
There has been a substantial impact of this PCN, details of such are as followed:
- ‘They have been identified by an independent audit on behalf of NHS England as an exemplar of best practice’
- ‘They use a 0365 platform to share project information and documentation. This has provided visibility of project progress and support collaborative and agile working in the absence of shared file arrangements- dedicated programme support’
- ‘Dedicated programme support has enabled the work to move at pace, providing a structure for everyone to feed into and embrace’
- ‘CSU expertise within the programme management provided valuable support in sharing best practice across the network, using case studies to support current and future opportunities in collaborative working’
- ‘created a robust governance structure has enhanced working relationships and provided visibility and clarity on roles and responsibilities across the network’
Their shared vision is: “Working together to deliver high quality, innovative and sustainable healthcare for our community with commitment, compassion and integrity”.
Successes of Primary Care Networks: Self Evaluation for Staff
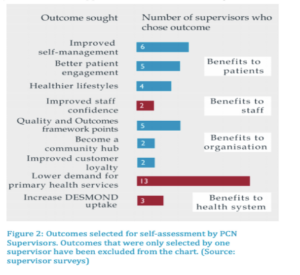
As exemplified by the National Association of Primary Care, Figure 2 presents the outcomes of a questionnaire for staff. It shows the self-assessment by PCN supervisors, of how networks have improved the workplace. As shown, there is a lower demand for primary health services and patients are engaging more and benefiting from healthier lifestyles.
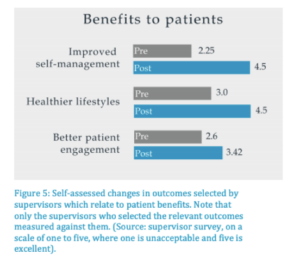
Figure 5 (as presented on NAPC.co.uk) also presents that improved self-management, healthier lifestyles and patient engagement has increased pre vs. post PCN.
Contact Our Team Today
If you need help on a tender, contact our experienced team of writers today on 0330 133 8823.
Alternatively, send an email to info@klowconsulting.com for more information and details.

